Colonoscopy
What is Colonoscopy?
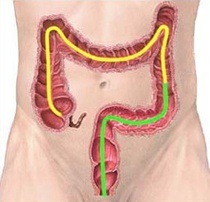
Colonoscopy is a procedure used to examine or inspect the inside surface of the large bowel, which also allows a variety of therapeutic procedures to be carried out through the instrument. Such procedures may include the taking of tissue samples (biopsies) and removal of polyps (benign wart like growths).
How are you prepared?
Prior to the examination you will be provided with a kit containing full instructions. If you have serious heart or chest problems or drug allergies, special precautions need to be taken to reduce any risk. You should therefore inform the doctor of any serious conditions of this nature. You should cease taking Iron tablets one week before test and if you are taking Warfarin or Plavix please discuss this with your doctor. For a few days prior to the procedure you will need to follow a low residue diet. The night before the examination you will need to take laxatives and further preparation, usually a quantity of salty tasting solution which completely flushes out the colon. You will be given sedation before the procedure begins and usually you will not remember anything about the examination.
What we do
The colonoscope is a long highly flexible tube about the thickness of your index finger. It is inserted through the rectum and allows inspection of the whole of the large bowel. Occasionally narrowing of the bowel or other diseases may prevent the instrument being inserted through the full length of the colon. As colon cancer arises from pre-existing polyps (benign tumours), it is advisable that if any polyps are found, they be removed at the time of examination. Most polyps can be burnt off by placing a wire snare around the base and applying an electric current.
Afterwards
You will be given time to recover from your procedure in an observed recovery area, during which time you will given a drink with biscuits.
The doctor will:
- Talk with you and discuss his findings
- Give you a hand-written report regarding your procedure and any follow up instructions
- Send a detailed report to your doctor
 For legal reasons you must not drive a vehicle or operate machinery for at least 12 hours following sedation. Driving under the influence of sedation carries the same implications as with alcohol. You should have a responsible adult with you to drive you home and stay with you for twelve hours.
For legal reasons you must not drive a vehicle or operate machinery for at least 12 hours following sedation. Driving under the influence of sedation carries the same implications as with alcohol. You should have a responsible adult with you to drive you home and stay with you for twelve hours.
The sedation you will be given is very effective in reducing any discomfort and although you will be awake relatively quickly afterwards, the effects of the sedation will remain in your system for up to 12 hours. For this reason, you will be unable to drive unit the next day after the procedure. Please have someone with you to drive you home and stay with you for 12 hours.
Risks and complications
For inspection of the bowel alone, complications of colonoscopy are very uncommon. Most surveys report complications of 1:1000 examinations or less.
Complications
Complications which can occur include an intolerance of the bowel preparation solution or reaction to the sedative used. Perforation (making a hole in bowel) or major bleeding from the bowel is extremely rare, but if it occurs may require surgery.
When operations, such as removal of polyps, are carried out at the time of procedure, there is a slightly higher risk of perforation or bleeding from the site where the polyp was removed.
Complications of sedation are uncommon and are usually avoided by administering oxygen during the procedure and monitoring pulse and oxygen levels in the blood.
A number of rare side-effects can occur with any endoscope procedure. If you wish to have full details of such complications explained to you please discuss this with the doctor prior to the examination.
Because of the risk of cancer, it is recommended that all polyps found be removed at the time of colonoscopy. Due to sedation, it will not be possible to discuss the removal at the time, therefore if you have any queries regarding polyp removal please discuss this prior to the procedure. In the unlikely event of haemorrhage occurring, blood transfusion may be necessary.
It is important to realize that no test is perfect and small lesions, and rarely even cancers, can be missed during colonoscopy. (The rate of missed cancer is 0.6 - 2/1000 patient years) For this reason, follow up colonoscopy is recommended and if there is a change in your symptoms, these should be discussed with your doctor even if you have previously had a colonoscopy.